It can be a challenge to keep up with the latest innovations in hospital ventilation systems and techniques, and the many ways they are changing the management of patients with respiratory failure. Staying up to date on emerging applications, including noninvasive ventilation (NIV) and high-flow therapy, is important given how many patients are ventilated during a hospital stay and the importance of weaning to reduce complications from continued breathing assistance.
50%+ of ICU patients are intubated within 24 hours of admission1

310 per 100,000 U.S. adults undergo invasive ventilation for nonsurgical indications2
40% of the total duration of mechanical ventilation is the weaning process3
NIV and high-flow nasal cannula: emerging applications
It’s no exaggeration to say that NIV has revolutionized the treatment of acute respiratory failure.4 And recently, high-flow nasal cannula (HFNC) oxygen delivery has gained popularity as part of a strategy for supportive therapy in many clinical situations, including weaning. Learn what experts are saying about these modalities.
Share with colleagues:
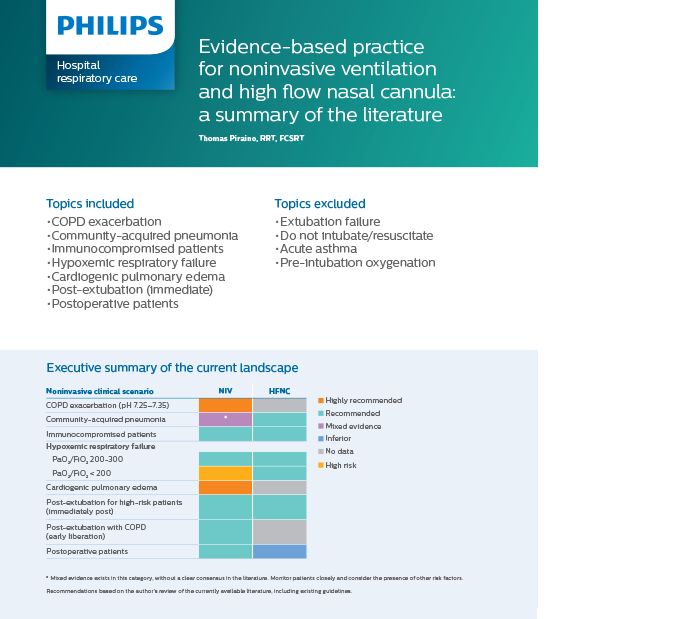
Read an evidence-based clinical summary of the literature
Share with colleagues:
Why NIV over invasive ventilation?
Clinicians understand that while invasive ventilation can be lifesaving, the risk of potential complications – like infections and injury to the lungs and other organs – runs high. That’s why NIV has become a widely used therapy option and is now considered the mode of choice for some conditions. NIV has also been associated with reduced length of hospital stay and reduces mortality, patient discomfort and length of-stay for exacerbations of COPD compared to standard therapy.5
Advantages of NIV over invasive ventilation
Application Minimize ventilator acquired pneumonia6 Decreases work of breathing
Oral patency
Transitioning to NIV?
Here are some tips: Set realistic expectations – NIV does not avoid intubation in all cases – a NIV failure rate of 20-40% is expected based on current clinical evidence.7 Experience matters – Only practice of NIV will lead to the needed experience to perform successful NIV.
Noninvasive ventilation is one of those rare medical technologies that both improves patient outcomes and reduces treatment costs.”
– Adam Seiver, MD, PhD, MBA, chief medical officer, Philips Monitoring and Analytics & Therapeutic Care
Share with colleagues:
Avoid NIV complications
Complications with NIV can be pressure-related
| Complication | Remedy8 |
| Nasal congestion | Try humidification or speak to the physician for various remedies to assist with this problem |
| Nasal or oral dryness | Add humidification, nasal saline, oral/nasal hygiene, or decrease leak |
| Sinus or ear pain | Lower inspiratory pressure |
| Gastric inflation | Avoid excessive inspiratory pressures (over 20 cmH2O) |
| Eye irritation | Check mask fit, readjust bottom headgear straps, and be aware of air leaks near eyes |
| Failure to ventilate | Use sufficient pressures, optimize patient-ventilator synchrony |
Complication
Nasal congestion
Remedy8
Try humidification or speak to the physician for various remedies to assist with this problem
Nasal or oral dryness
Try humidification or speak to the physician for various remedies to assist with this problem
Sinus or ear pain
Lower inspiratory pressure
Gastric inflation
Avoid excessive inspiratory pressures (over 20 cmH2O)
Eye irritation
Check mask fit, readjust bottom headgear straps, and be aware of air leaks near eyes
Failure to ventilate
Use sufficient pressures, optimize patient-ventilator synchrony
Complication
Nasal congestion
Remedy8
Try humidification or speak to the physician for various remedies to assist with this problem
Complication
Nasal or oral dryness
Remedy8
Try humidification or speak to the physician for various remedies to assist with this problem
Complication
Sinus or ear pain
Remedy8
Lower inspiratory pressure
Complication
Gastric inflation
Remedy8
Avoid excessive inspiratory pressures (over 20 cmH2O)
Complication
Eye irritation
Remedy8
Check mask fit, readjust bottom headgear straps, and be aware of air leaks near eyes
Complication
Failure to ventilate
Remedy8
Use sufficient pressures, optimize patient-ventilator synchrony
Complications can also be mask-related
| Complication | Remedy8 |
| Discomfort | Check fit, adjust straps, or change the mask |
| Nasal or oral dryness | Add humidification, nasal saline, oral/nasal hygiene and manage leak by decreasing the amount of leak |
| Nasal bridge redness or ulceration | Use an artificial skin, minimize strap tension, use LiquiCell, alternate masks or use a PerforMax or Total face mask |
| Skin irritation or rashes | Use a skin barrier lotion and/or topical corticosteroids, change to a mask made from a different material, be sure to properly clean the mask |
| Claustrophobic reactions | Try a nasal mask or |
Complications can also be mask-related
Complication
Remedy8
Discomfort
Check fit, adjust straps, or change the mask
Nasal or oral dryness
Add humidification, nasal saline, oral/nasal hygiene and manage leak by decreasing the amount of leak
Nasal bridge redness or ulceration
Use an artificial skin, minimize strap tension, use LiquiCell, alternate masks or use a PerforMax or Total face mask
Skin irritation or rashes
Use a skin barrier lotion and/or topical corticosteroids, change to a mask made from a different material, be sure to properly clean the mask
Claustrophobic reactions
Check mask fit, readjust bottom headgear straps, and be aware of air leaks near eyes
Complications can also be mask-related
Complication
Discomfort
Remedy8
Check fit, adjust straps, or change the mask
Complication
Nasal or oral dryness
Remedy8
Add humidification, nasal saline, oral/nasal hygiene and manage leak by decreasing the amount of leak
Complication
Nasal bridge redness or ulceration
Remedy8
Use an artificial skin, minimize strap tension, use LiquiCell, alternate masks or use a PerforMax or Total face mask
Complication
Skin irritation or rashes
Remedy8
Use a skin barrier lotion and/or topical corticosteroids, change to a mask made from a different material, be sure to properly clean the mask
Complication
Claustrophobic reactions
Remedy8
Check mask fit, readjust bottom headgear straps, and be aware of air leaks near eyes
Did you know?
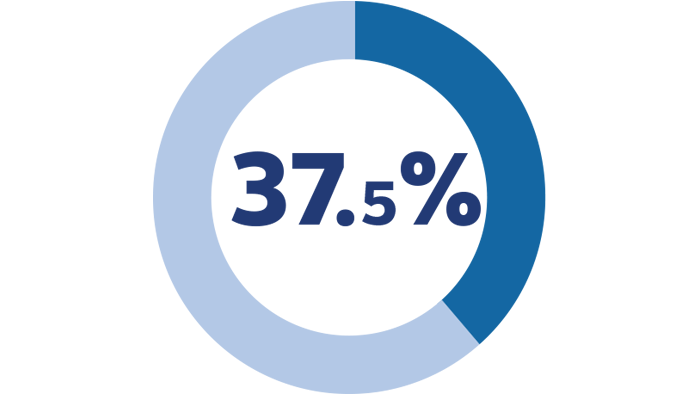
37.5% of patients fail NIV because of mask intolerance and discomfort, a reason recognized as one of the most common for NIV failure. This is because the mask was not fitted properly or it’s the wrong type of mask for the patient.9
Education and resources
Explore webinars, courses and videos for practice guidelines and ways to enhance your hospital ventilation program’s success.
Skin integrity training LeBonheur Children’s Hospital and Philips team up to bolster staff education through Philips Saving Face NIV mask rotation training program.
HFNC and NIV current and practice This presentation reviews evidence in support of NIV and discusses the research evaluating HFNC and its role in the management of respiratory failure.
Optimal respiratory care requires optimal technique High-flow oxygen therapy (HFT), noninvasive ventilation (NIV) and invasive mechanical ventilation (IMV): Understanding which technique is appropriate and when, can help improve patient care and assist clinical teams for success.
References 1. According to the American Association for the Surgery of Trauma (AAST). 2. Mehta AB, Syeda SN, Wiener RS, Walkey AJ. Epidemiological trends in invasive mechanical ventilation in the United States: a population-based study. J Crit Care. 2015;30(6): 1217-1221. 3. McConville JF, Kress JP. Weaning patients from the ventilator. N Engl J Med. 2012;367(23):2233-2239. 4. Scott K. Epstein, MD, Respiratory Care, January 2009 Vol 54 No 1. 5. Keenan SP, Gregor J, Sibbald WJ, Cook D, Gafni A. Noninvasive positive pressure ventilation in the setting of severe, acute exacerbations of chronic obstructive pulmonary disease: more effective and less expensive. Crit Care Med. 2000 Jun;28(6): 2094-102. 6. Respiratory Care, Feb 2009 54(2):198-211) 7. Hess D. How to Initiate a Noninvasive Ventilation Program: Bringing the Evidence to the Bedside. Respiratory Care (2009), Vol 54 NO 2: p. 232-245. 8. Nava, S., et al. Interfaces and Humidification for Noninvasive Mechanical Ventilation. Resp. Care. Jan 2009. Vol 54-1. 9. Squadrone E, et al. Noninvasive vs invasive ventilation in COPD patients with severe acute respiratory failure deemed to require ventilatory assistance. Inten Care Med. 2004;30(7). Philips is not a medical care provider, and this information is not intended to diagnose, examine treat or manage medical conditions of any kind. The content on this page is not a substitute for professional judgment by a healthcare provider.
