A personalised asthma action
A personalised asthma action plan (also known as a treatment plan) is a written plan designed by you and your healthcare professional that provides instructions on how to control you or your child’s asthma.1 Because everyone’s asthma symptoms and triggers maybe different, the action plan should be personalised or customised to the individual’s asthma. Contact your healthcare professional and set up an appointment to develop an asthma action plan for yourself or your child. Before you start managing asthma, it is important to understand a little more about you or your child’s asthma. What are your early warning signs, symptoms, and triggers? This information should be recorded in a diary or an asthma app. Keep a diary either on paper or electronically to record the following:
Common asthma triggers
Triggers may be unique to each individual who has asthma.2 Common triggers include: It is important to track not only trigger exposure, but also if symptoms occur1 so that you and your healthcare professional can develop a trigger control plan. This would be useful information to help you and your healthcare professional to not only identify asthma triggers but the information may be used to develop a trigger control plan. These personal triggers and control plan for management of triggers should be listed on the asthma action plan. Managing your indoor air quality may help in managing allergens and triggers.

Symptoms and early warning signs
It will also be helpful to identify symptoms and early warning signs. Examples of symptoms are waking at night, coughing, wheezing, chest tightness, or shortness of breath during exercise. Symptoms are also unique to each person. Not all individuals who have asthma wheeze. In some cases, the only symptom may be a cough3. The asthma action plan should have a place to list personal symptoms and step-by-step instructions regarding how to manage symptoms.
Peak flow readings
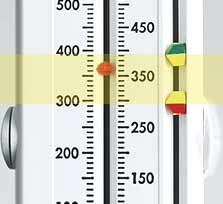
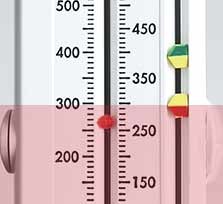
The peak flow reading is a measure of how fast you can blow out the air in your lungs using a peak flow meter. Just like triggers and symptoms, a peak flow reading may be unique to anyone who has asthma. Therefore, when using a peak flow meter it is important to determine you or your child’s personal best peak flow reading. A personal best peak flow reading is the highest reading that can be achieved when asthma is controlled. To determine personal best, measure peak flow readings for two weeks twice a day, write these down in a peak flow chart and share these readings with your healthcare professional. Because different peak flow meters may provide slightly different readings, it is important you use the same peak flow meter. Your healthcare professional can use these readings to determine you or your child’s personal best peak flow reading. They can then create a personalised asthma action plan for you. This reading will be used by your healthcare professional to help develop a personalized written asthma action plan.
Understanding the zones in an asthma action plan
Your healthcare professional may use the information you recorded in your diary regarding asthma triggers, peak flow readings, symptoms and early warning signs to develop a personalised written asthma action plan using the zone system. He or she will teach you to use the zone system to assess the severity and frequency of asthma symptoms, changes in peak flow readings and how to follow their instructions for use of asthma medications. The zones and written instructions from your healthcare professional will be laid out in the asthma action plan like a traffic light: Green means that asthma is in good control. You or your child are symptom-free and peak flow readings are 80-100% of the personal best reading. You can GO ahead with regular activities. In the green zone, the medication instructions provide details how to take daily controller medications.
The three zones of asthma management are part of an asthma action plan. The zones are a simple colour-coded system to help patients and parents of children with asthma to recognise the severity of asthma symptoms and changes in peak flows, so that they can use their asthma medications at the right time and deliver the correct amount of medication. The instructions in the zone system are set up like a traffic light which makes it simple to understand.
Yellow means symptoms are present, peak flow readings are 50-80% of personal best reading. You should proceed with CAUTION. The yellow zone, contains instructions regarding how often to use the reliever medications and when to call your healthcare professional.
Red means that you or your child are having severe symptoms and peak flow readings are less than 50% of personal best reading. You should STOP and get medical attention. The red zone contains instructions regarding the immediate use of reliever medications and instructions to call the healthcare professional immediately or alternatively to call 999.
PersonalBest peak flow meter zones
Many peak flow meters have zone indicators that can be set by the healthcare professional on the peak flow meter. Once these are set, the indicator will point to the green, yellow or red zone which will allow you to quickly evaluate where your or your child’s peak flow reading fall within the zones. You can then refer to the written personalised asthma action plan and follow the instructions provided by your healthcare professional for how to take asthma medications.

Green zone
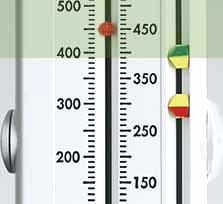

Yellow zone

Red zone
Why is an asthma action plan so helpful
Still not sure exactly how an action plan makes such a difference. You can use it to:
What if my asthma changes - won't the plan go out of date? Your asthma action plan should be reviewed and updated at least once a year at your asthma review with your doctor.1 You need to remember to take it with you to every asthma appointment - including any emergency or consultant visits - so that if there are any changes to the way you need to look after your asthma, your plan can be updated. It is also useful for hospital staff to be able to glance at the information in your action plan, especially if you are finding it difficult to talk due to your symptoms.2
Be prepared
Keep a list of emergency contact numbers. It is important to list the healthcare professional's phone number and emergency phone numbers on the action plan. If the action plan is for your child, make sure you list your mobile phone number. Preparation is the key to success. Once you have a personalised asthma action plan, put a plan in place for using it. Keep the action plan in a handy place so you can act quickly. Keep a copy in a readily available place in your home – such as posted on your refrigerator. Just like the reliever medication make sure you have a copy with you when you travel away from home. Keep a copy in your purse, backpack or wallet so you can have immediate access to it. Review it with all that are involved in care. This includes your entire family members so they know what to do in case of an emergency. If the action plan belongs to your child, provide a copy to the schools and review it with your child’s teachers and coach. Keep the action plan up-to-date. Asthma symptoms, triggers and medications may all change over time. Keep regular check-ups with the healthcare professional and adjust the action plan as needed.
Frequently asked questions

Sign up to for more information from Philips
Are you a healthcare professional?
DISCLAIMER:
Information on this website is informational only and should not replace the advice of a physician.
FOOTNOTES: [2] asthma.org.uk/advice/manage-your-asthma/action-plan. Accessed October 2017. [3] Webmd.boots.com. Asthma/guide/asthma-symptoms. Accessed Nov 2017.
[1] mayoclinic.org/diseases-conditions/asthma/in-depth/asthma/art-20044888. Accessed October 2017.

